Choosing Wisely
The Choosing Wisely Strategic Advisory Group is an initiative ignited by the broader campaign led by the ABIM Foundation. The overarching aim is been to ignite conversations between clinicians and patients regarding the necessity of tests, treatments, and procedures. Originating in 2012 with nine national specialty societies representing 375,000 clinicians, the campaign initially presented 45 examples of commonly utilized tests or treatments lacking strong supporting evidence.
Over the years, this initiative has evolved, with more than 80 specialty societies contributing additional examples until 2023. Societies, like EAP, have been encouraged to publish individual lists.
The CW SAG of EAP was established in 2018 and is consisting of active 32 members from 19 European countries.
For Physicians
For Parents

ENGLISH
CZECH

FINNISH

FLEMISH / DUTCH
FRENCH
GERMAN

ITALIAN

NORWEGIAN
PORTUGUESE

SLOVENIAN

SPANISH
For Physicians
Top 10 Recommendations
Cough Medication
Do not recommend, prescribe or use cough medicines in children.
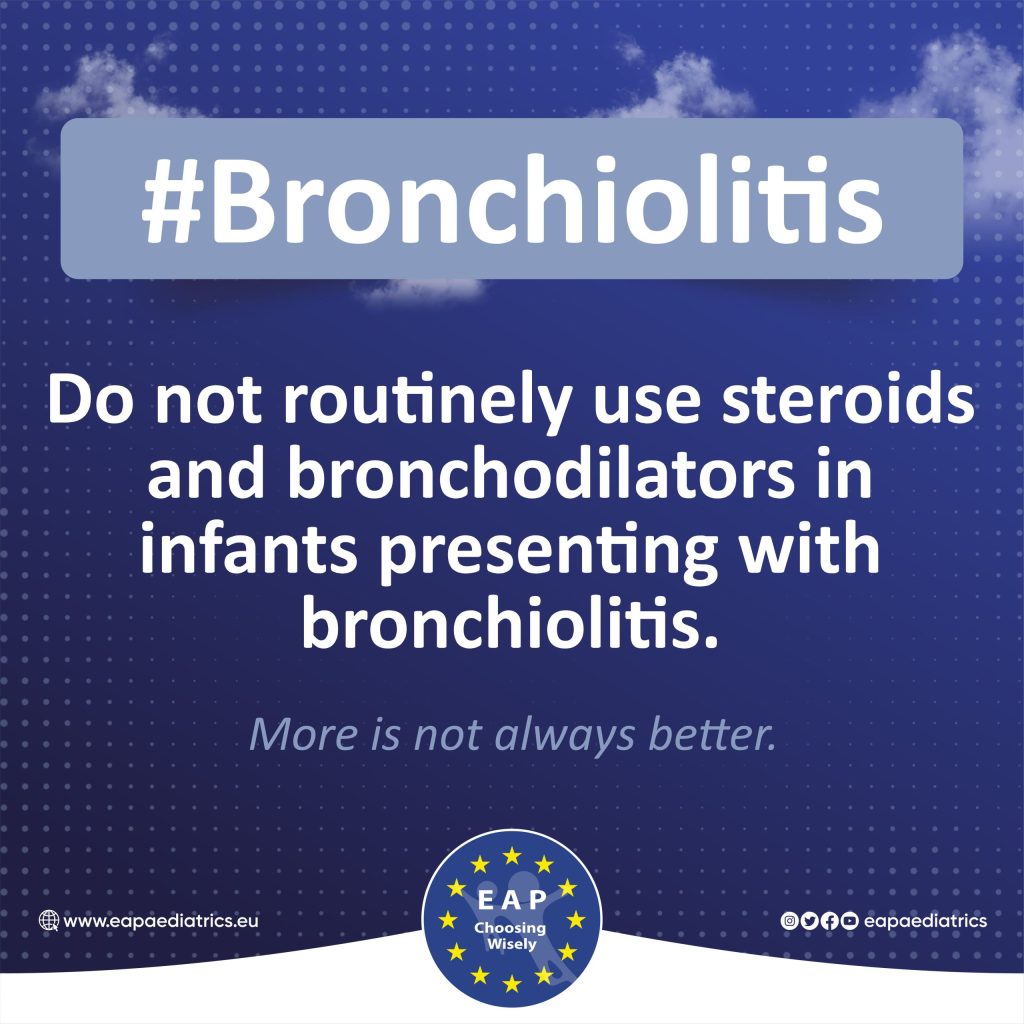
Bronchiolitis
Do not routinely use steroids and bronchodilators in infants presenting with bronchiolitis.
IV-Antibiotic Duration
Duration: Do not routinely prolong IV antibiotics to treat severe infections, but consider switching to the oral form as soon as the clinical condition has improved.
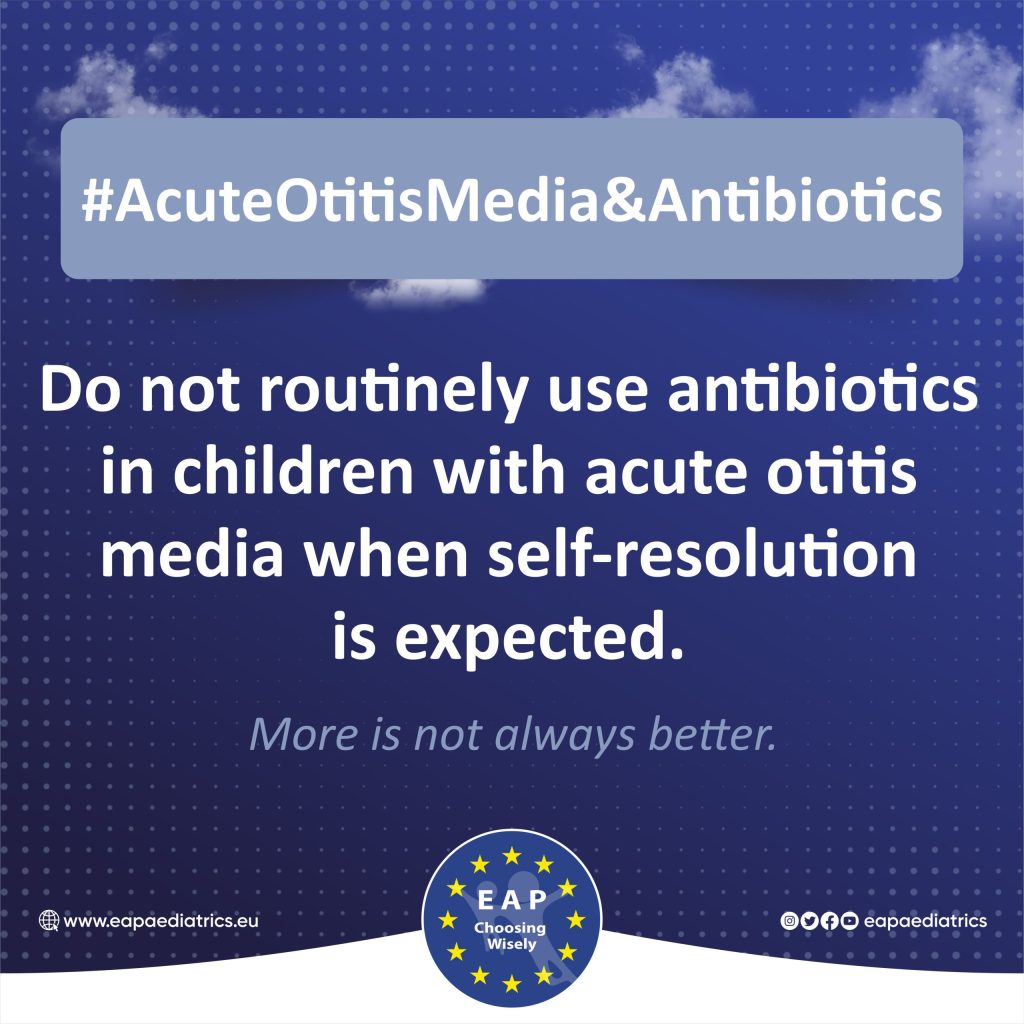
Acute Otitis Media & Antibiotics
Do not routinely use antibiotics in children with acute otitis media when self-resolution is expected.
Antibiotics in Neonates
Do not prescribe antibiotics for neonates without clinical signs of sepsis.
Hospitalization of Febrile Infants
Do not routinely continue hospitalization in well-appearing febrile infants once bacterial cultures have been confirmed negative for 24 to 36 hours if adequate outpatient follow-up can be assured.
Duration of Neonatal Antibiotics
Do not continue antibiotic therapy for suspected neonatal sepsis >36-48 hours without clear suspicion of bacterial infection.
IgE Testing
Do not perform screening panels (IgE tests) for food allergies without a history consistent with a specific food allergy.
Urine Culture
Do not request urine culture in febrile children older than 2 months with respiratory tract infection.
Gastroesophageal Reflux
Do not routinely prescribe acid blockers and motility agents in infants with GER.
For Parents
Top 10 Recommendations
Cough Medication
Do not recommend, prescribe or use cough medicines in children.
Bronchiolitis
Do not routinely use steroids and bronchodilators in infants presenting with bronchiolitis.
IV-Antibiotic Duration
Duration: Do not routinely prolong IV antibiotics to treat severe infections, but consider switching to the oral form as soon as the clinical condition has improved.
Acute Otitis Media & Antibiotics
Do not routinely use antibiotics in children with acute otitis media when self-resolution is expected.
Antibiotics in Neonates
Do not prescribe antibiotics for neonates without clinical signs of sepsis.
Hospitalization of Febrile Infants
Do not routinely continue hospitalization in well-appearing febrile infants once bacterial cultures have been confirmed negative for 24 to 36 hours if adequate outpatient follow-up can be assured.
Duration of Neonatal Antibiotics
Do not continue antibiotic therapy for suspected neonatal sepsis >36-48 hours without clear suspicion of bacterial infection.
IgE Testing
Do not perform screening panels (IgE tests) for food allergies without a history consistent with a specific food allergy.
Urine Culture
Do not request urine culture in febrile children older than 2 months with respiratory tract infection.
Gastroesophageal Reflux
Do not routinely prescribe acid blockers and motility agents in infants with GER.
Booklet
Countries Involved
Contact